Paul S. Sidhu BSc MB BS MRCP FRCR DTM&H FAIUM(Hon.) EFSUMB President Elect (2015 – 2017)
Professor of Imaging Sciences, King’s College London, Department of Radiology, King’s College Hospital, London, United Kingdom.
How to use CEUS as a problem solving tool in clinical practice?
A series of case studies for best practice.
- Prof. Paul S. Sidhu EFSUMB President Elect (2015 – 2017)
Introduction
A B-mode sonographic examination is normally the first line investigation in a number of clinical scenarios in the assessment of upper abdominal symptoms, and often the first line investigation of an abnormal liver function biochemical profile. A primary care physician is frequently the initiator of the sonographic investigation and will respond appropriately to the findings, which may include a suggestion for further imaging and management. It is important to appreciate the sonographic examination is almost certainly performed without the addition of a contrast agent, unlike a Computed Tomography (CT) examination where it is rare not to perform the examination without a contrast agent, inherently an iodine-based agent with a known risk profile.
Furthermore, the CT examination involves a radiation dose, an important issue with the younger patient, as an accumulative radiation dose potentiates malignancy1,2.
When an incidental focal liver lesion is found on the sonographic examination, it is difficult to be absolutely confident of the nature of the lesion without further imaging or sonographic follow-up3. Nevertheless, in patients referred from the community or without known underlying primary malignancy elsewhere, a focal lesion in the liver is benign nearly 80% of the time4.
The ideal situation at the time of the discovery of the focal liver lesion during the sonographic examination would be to correctly inform the patient of the nature of the lesion, benign in most cases, and to relieve anxiety. If the focal liver lesion is malignant, appropriate management can be instituted rapidly. The introduction of microbubble contrast agents has improved the characterization of focal liver lesions to such a level to rival CT and Magentic Resonance (MR) imaging5 recognized in current guidelines6.
The addition of a microbubble contrast agent immediately, as an adjunct to the B-mode sonographic examination has tremendous benefits in terms of diagnosis, alleviating patient anxiety, planning of management and is also cost-effective7.
Although the administration of the microbubble agent needs the insertion of an intravenous line, and a second trained person to inject the agent, the whole examination requires no more than 5 minutes of extra examination time.
The microbubble contrast agent used most often in Europe and Asia for the detection and characterization of focal liver lesions is SonoVue™/Lumason™ (Bracco, SpA, Milan). It has an excellent safety profile, with an adverse incident rate of 0.0086%8.
A series of incidentally discovered focal liver lesions are detailed, where the addition of a microbubble agent has facilitated the management of the patient, with little disruption to the management of the workflow of the sonographic department.
A 38-year-old male patient was referred from his primary care physician with a feeling of “fullness” following a meal, some weight loss and upper abdominal discomfort, intermittent in nature. There was no relevant past medical history. Clinical examination was unremarkable, but a “mass” was palpated in the upper central abdominal area. An urgent sonographic examination was requested.
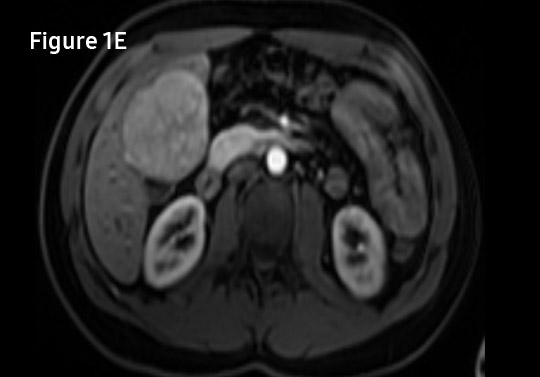
The sonographic findings on the contrast-enhanced ultrasound (CEUS) were diagnostic for an area of Focal Nodular Hyperplasia (FNH). The patient was reassured that the abnormality was benign and the appropriate referral to a hepatologist was initiated. A subsequent MR examination was in keeping with the diagnostic CEUS examination.
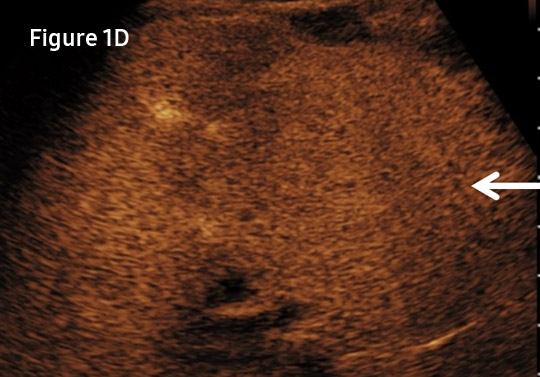
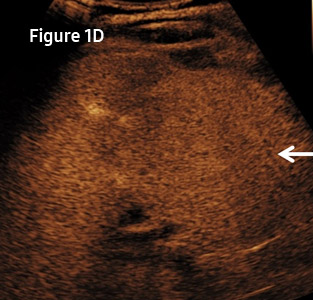
A 45-year-old female patient was referred by a primary care physician, with symptoms of vague abdominal discomfort, precipitated by food. The past medical history was not relevant to the current symptoms, but included previous inguinal hernia repair. There was a family history of gallstones. The patient was referred for a sonographic examination for the investigation of possible gallstones as a cause for symptoms.
On the B-mode examination, a hypoechoic lesion was identified in a fatty liver, with no characteristics of note. On the CEUS examination, there is peripheral globular enhancement with gradual in-filling of the lesion over time; features characteristic of an atypical hemangioma. In this patient there was complete in-filling, but some hemangioma will never fill completely. No further imaging was needed. A follow-up sonographic study in 3 months showed no change in appearances.

- Figure 2A. A 2.48 cm hypoechoic lesion (between cursors) lying at the lower aspect of the left liver lobe does not have the sonographic characteristics of a hemangioma, but is present in a fatty liver.
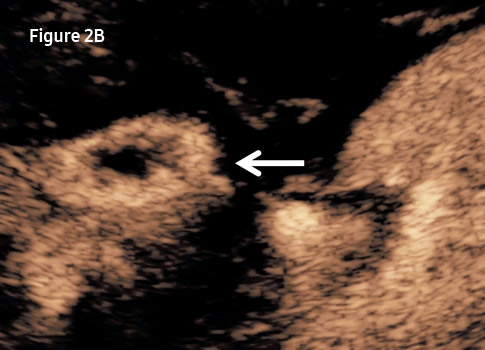
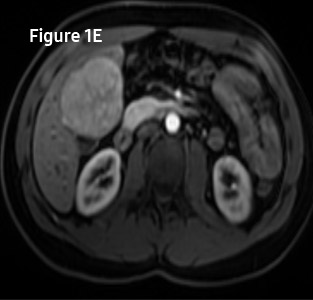
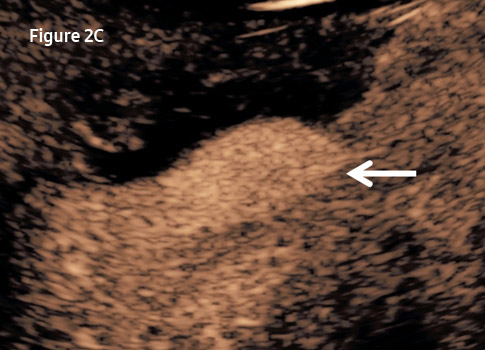
- Figure 2B. Following injection of 2.4 ml of SonoVue™/Lumason™ (Bracco, SpA, Milan), at 27 seconds, the early portal venous phase, there is globular peripheral enhancement of the lesion (arrow).
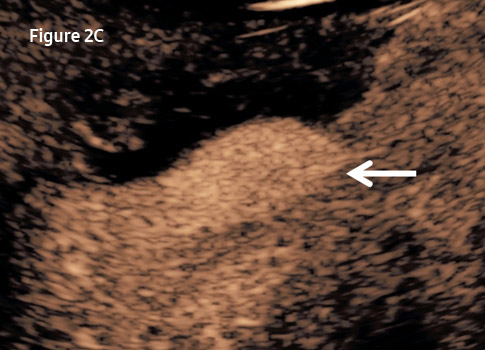
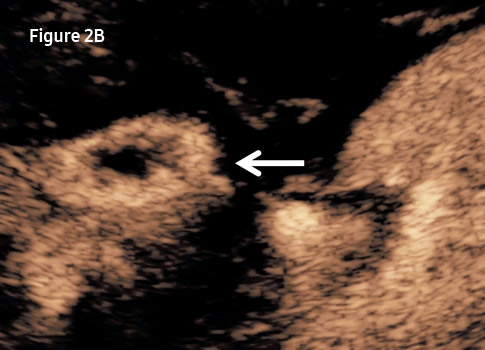
- Figure 2C. At 86 seconds, there is complete in-filling of the lesion (arrow), characteristic of a hemangioma.
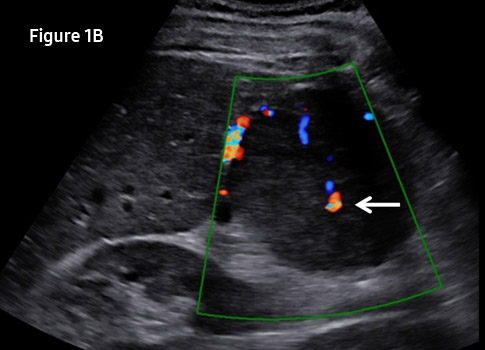
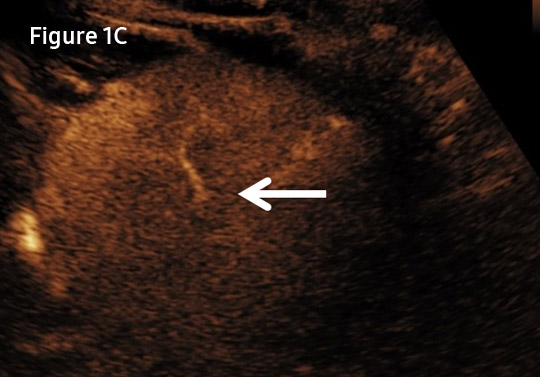
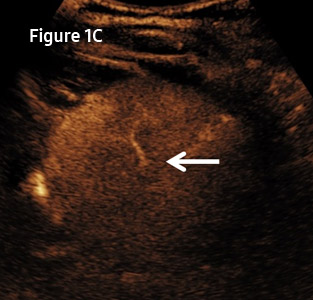
An 85-year-old male patient was assessed on a routine follow-up sonographic examination for known underlying treated colorectal malignancy, 5-years previously. There was underlying well-controlled congestive cardiac failure, no other medical history of note. An incidental “target” lesion was seen in segment 5 of the right liver lobe, which was not present on a sonographic examination 6 months previously.
A CEUS examination was performed with intense vascularization and rapid “wash-out” of the lesion, characteristic of a focal malignant lesion, and likely a metastases. A sweep through the liver in the late portal venous phase, looking for focal areas of wash-out (“black holes”), designed to detect any further metastatic deposits was negative. A biopsy was performed, confirming metastatic adenocarcinoma, with response to percutaneous ablation.
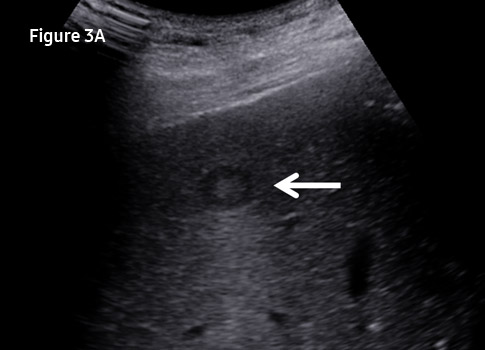
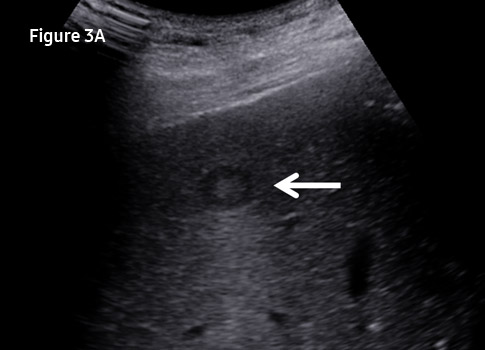
- Figure 3A. On the B-mode sonographic examination, a well-circumscribed lesion of mixed echogenicity is seen (arrow), appearances suggesting a “target” lesion from colorectal primary malignancy.
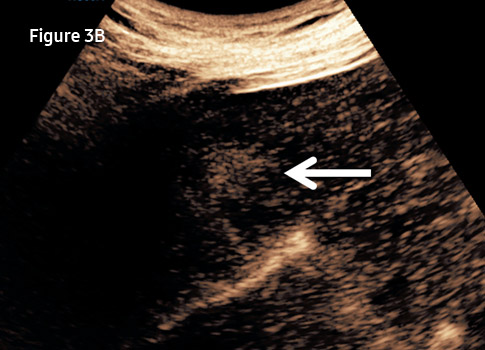
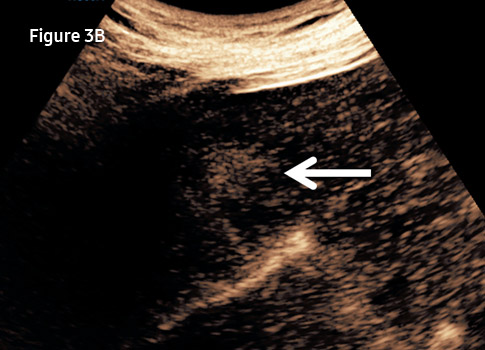
- Figure 3B. Following injection of 2.4 ml of SonoVue™/Lumason™ (Bracco, SpA, Milan), at 35 seconds, the arterial phase in the presence of heart failure, the lesion is hyper-enhancing in comparison to the background liver, in keeping with a vascular lesion (arrow).
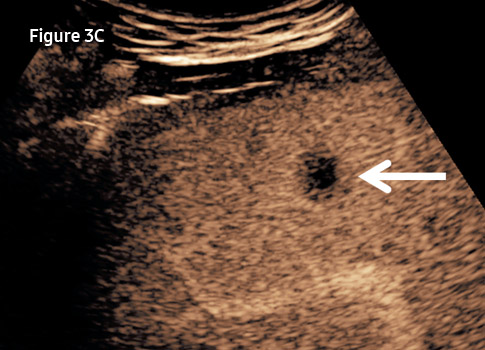
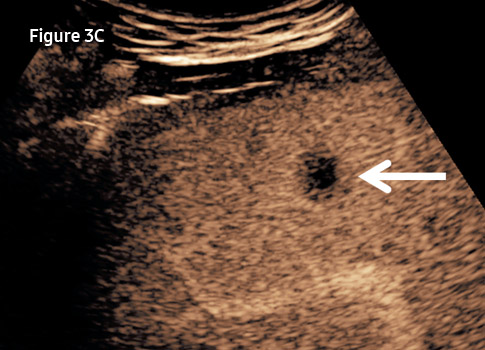
- Figure 3C. At 105 seconds, in the late portal venous phase, there is “wash-out” of the lesion (arrow) confirming the malignant nature and likely a metastatic deposit from the primary colorectal malignancy.
Supported Systems
- - RS80A with Prestige
Reference
-
- Brenner DJ, Hall EJ. Cancer risks from CT scans: now we have data, what next? Radiology 2012;265:330-1.
- Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol 2008;81:362-78.
- Willits I, Burn J, Cole H, Hoare T, Sima A. What proportions of focal liver lesions detected by unenhanced ultrasound are inconclusive? Ultrasound 2015;23:78-84.4.
- Bartolotta TV, Taibbi A, Midiri M, Matranga D, Solbiati L, Lagalla R. Indeterminate focal liver lesions incidentally discovered at gray-scale US. role of contrast-enhanced sonography. Invest Radiol 2011;46:106-15.
- Seitz K, Bernatik T, Strobel D, Friedrich-Rust M, Strunk H, Greis C, et al. Contrast- enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI - a prospective comparison in 269 patients. Ultraschall in Med 2010;31:492-9.
- Claudon M, Dietrich CF, Choi BI, Kudo M, Nolsoe C, Piscaglia F, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver - update 2012. Ultraschall in Med 2013;34:11-29.
- Leen E, Moug S, Horgan P. Potential impact and utilization of ultrasound contrast media. Euro Radiol Suppl 2004;14:P16-P24.
- Piscaglia F, Bolondi L. The safety of SonoVue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound in Med Biol 2006;32:1369-75.
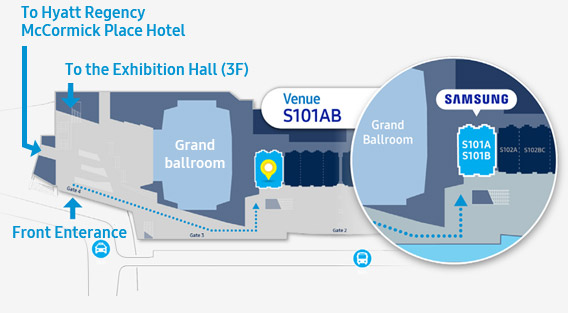
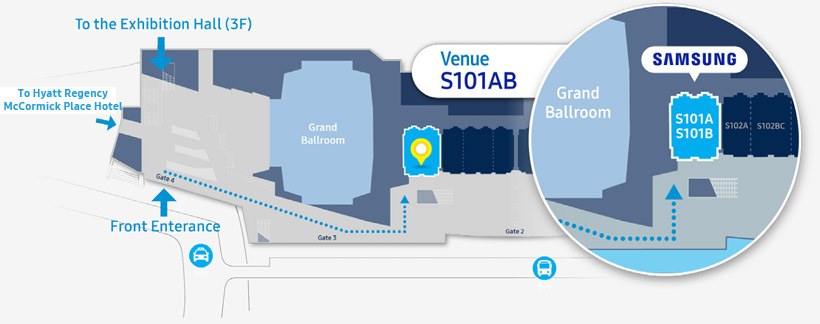
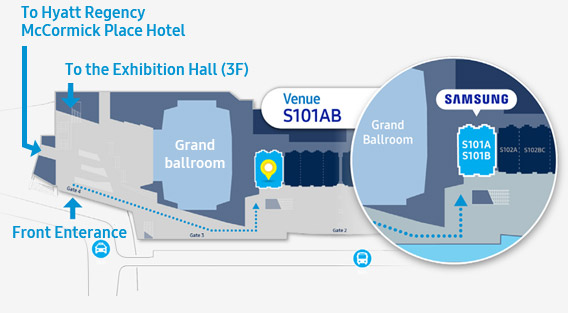
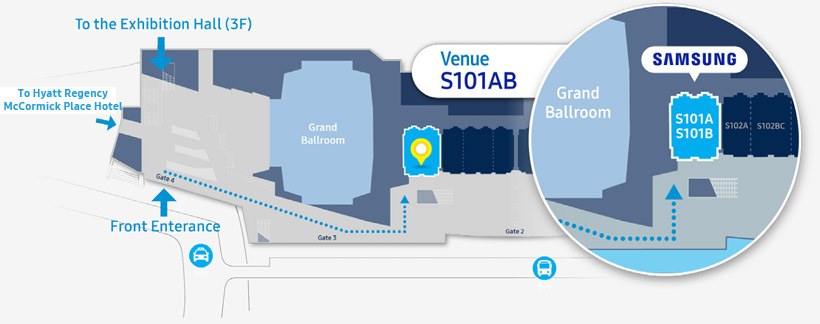
RSNA 2016
Samsung CEUS
Symposium
- Date
- Monday, Nov 28
- Time
- 08:30 - 10:00 AM
- Venue
- S101AB
McCormick Place,
Ground floor 1F
TOPIC
-
How to Incorporate CEUS into your Imaging Practice
| Time |
Title |
Speaker |
| 08:30 - 09:00 |
CEUS as a problem solving tool in clinical practice |
Prof. Paul Sidhu |
| 09:00 - 09:30 |
Hepatocellular Carcinoma: The Advantages of Imaging with CEUS |
Dr. Stephanie R Wilson |
| 09:30 - 10:00 |
Efficacy and limitations of multiparametric ultrasound (CEUS, Color-doppler, S-Detect and 3D Arterial Analysis) in evaluation of carotid stenosis and thyroid nodules |
Dr. Prof. Vito Cantisani |
MAP &Directions
-
McCormick Place, Ground Floor 1F